Evolution of Medical Ethics and Bioethics in Greece: “Ancient-Christian-Contemporary Greece”
8 September 2016by Nikolaos Koios[1], Lambrini Veloyanni[2], Demetrios Alvanos[3]
Article published in “ELEFTHERNA” – SCIENTIFIC YEARBOOK – Vol III – 2006, Department of Psychology, School of Social Sciences, University of Crete
Summary
Although its authenticity has been questioned, the text that has been known as Hippocrates Oath has played a crucial role to the evolution of medical ethics in Greek settings. The Oath has influenced greatly Greek ethical thinking not only during antiquity, but also during early Christian times and Byzantine era. During the period of Turkish occupation the Oath recurs in Greece, in the texts of the Greek Enlighters. In modern times we trace it as the Oath taken by graduate students of Medicine, while it still serves as a basis for debates concerning the modern challenges of Bioethics and Medicine.
Key-words : Medical ethics, Bioethics, professional ethics, Hippocratic Oath, doctor – patient relationship, benefit for the patient, Christian anthropology
General
The appearance of medical ethics is almost coincident with the beginnings of medical science. In antiquity many societies obliged physicians to bind themselves to practise their profession in a proper and ethical manner, frequently by taking an oath. Every culture and every social system can show a framework for defining health, illness, therapeutic methods and doctors’ behavior, and understandably these commitments acquired an ethical aspect from the prevailing morality. In ancient Greece, and especially from the classical period onwards, it seems that the Greeks associated this most important science or calling with those ethical rules that would enable them to serve their fellow man in the best possible way (Jones, 1924).
After the Nuremberg trials, which led to a resurgence of interest in medical ethics in response to the atrocities perpetrated supposedly in the name of science, there was no noticeable rise in wider interest in the field. The appearance of bioethics in recent years has, however, rekindled interest in medical ethics.
Before proceeding with our review of the evolution and history of medical ethics and bioethics in Greece, the main concern of this paper, it may be useful to consider the distinction between medical ethics and bioethics.
Medical ethics is that branch of ethics which deals with the ethical problems arising from the practice of the medical profession. In other words it delimits the sphere of activity of the doctor, so he will not misuse or exploit the power he possesses by reason of his profession to the detriment of his patients. Thus medical ethics particularly focuses on the doctor-patient relationship.
Bioethics, on the other hand, is a modern interdisciplinary field dealing with the ethical problems arising fro the use of modern biomedical techniques. In brief, the basic bioethical issues are euthanasia, transplants, assisted reproduction, genetic modification, prenatal screening, genetic screening of adults and cloning. Bioethics is concerned with the very mechanisms of life, in the sense that humankind can now meddle with life in ways which until recently were inconceivable, and thus change the natural development of living things. Hence the field of bioethics includes interventions in the phenomenon of life, in psychosomatics, and in the environment. Perhaps at first glance one could say that bioethics examines practice rather than the practitioners, whereas medical ethics does the opposite. However, it cannot be denied that in bioethics too a role is played by the human factor, which is not always the doctor; it may be a geneticist or a biomedical technician.
Nevertheless, biomedical techniques are mostly used in clinical medical practice, so we inevitably return, though in a more complex way, to the doctor-patient relationship. In this case bioethics overlaps medical ethics to such an extent that almost all the concerns of the latter are subsumed under the former. For example, major questions of medical ethics, like doctors’ paternalism, patients’ rights, access to medical care and experiments on patients, are now examined within the framework of bioethics, to the extent that they are often referred to as purely bioethical issues.
Perhaps the best example of this is the question of informed patient consent. At bottom, informed consent can be seen as a question of medical ethics, of professional ethics and as a legal matter. With informed consent, an effort is made fully to acquaint the patient with the risks, the chances of success or failure, the moral issues and anything else that may interest him in connection with whatever medical or biomedical procedure he is about to undergo. The doctor or whoever else is to perform the procedure draws up a document, which the patient reads and after expressing his views or reservations signs if he accepts the proposed treatment. This description of informed consent would place it more readily in the field of medical ethics. However, because it is used universally in biomedical applications, it is classified and studied as a matter for bioethics.
From the above it can be seen that today the dividing line between bioethics and medical ethics is in practice blurred, and will in the future become even more so as biomedical techniques are used more widely in medical clinical practice. If, however, we wish to review the history of medical ethics and bioethics, we must begin by stating that historically they are two distinct fields. Medical ethics, as mentioned earlier, has existed since the birth of medical science in antiquity, whereas bioethics is the child of the last few decades of modern Western society. The roots of the former lie in the very beginnings of scientific and philosophical thought; those of the latter in the spirit and philosophy of Western modernism and postmodernism.
Examining the historical development of these two cultural phenomena in Greece, we can say that medical ethics, as it has come down to us, provided the foundation for bioethics. It is thus of great importance to examine the historical development of medical ethics in Greek civilization. Through the study of ‘old and familiar’ medical ethics, it will be easier to understand how modern Greek society confronts and incorporates ‘modern and imported’ bioethics. For this reason we have chosen to study the history of these two branches in Greek society separately.
Medical Ethics among the Ancient Greeks – Hippocratic Oath.
When considering medical ethics[4] in Classical Greece, and later on in Hellenistic and Roman-Greek society, we must stress certain points:
- Never in the Classical world was there a system of medical licensing. Anyone who undertook to treat patients could call himself a physician.
- There were no professional rules whatsoever with sanctions against physicians who violated professional ethics.
- It is misleading even to speak of professional ethics. At no time were physicians asked to take any oath, nor were they obliged to observe any code of ethics, formal or informal.
- However, ethical standards do appear in literature. But those that are more appealing to us, either because they can be regarded as timeless ideals of medicine or because they comply with modern medical ethics, could perhaps not always be applied by the majority of physicians.
- Even when certain ethical precepts are identified as ideals, at least for us, although not necessarily typical for that time, it should be noted that from Homer to Constantine the Great (9th century B.C. – 4th century A.D.) or, for that matter, from Hippocrates to Galen (5th century B.C.?-2nd century A.D.), there was not one period when they were constant.
- Medicine was certainly practised in the Hellenic world long before the time of Hippocrates, but due to the influence on the Western medical tradition of the “Father of Medicine” and the Oath that bears his name, the parts of the Hippocratic Corpus relating to medical ethics will serve as a central reference point in this article (Ammudsen & Ferngren, Gary B, 1983, pp. 1-46) .
Many students of the Hippocratic Corpus, Hippocratists as they are usually known, have put forward a variety of theories concerning the authorship of the texts. The historico-literary method has disclosed elements and influences that according to these researchers do not echo the spirit of the age of Hippocrates, nor the philosophical school to which he belonged, as revealed by the majority of the works that have been confirmed as his. Doubt has even been cast on his authorship of the Oath itself, the earliest Greek statement of medical ethics.
The basis for doubting – partially at least – the authorship of the Hippocratic Oath, is the discovery by the leading Hippocratist Ludwig Edelstein that many parts of the Oath reflect Pythagorean rather than Hippocratic philosophy (Edelstein, 1943). The two major medical schools of antiquity, those of Cos and Cnidus, partook of the all-pervading philosophical climate of Plato and Aristotle. Nicomachos, doctor and father of Aristotle, was a student of the Cnidus school (Marketos, 2002, p. 81). The Platonic and Aristotelian writings take positions that differ considerably from those of the Oath, for example on abortion. Both Plato and Aristotle permit abortion under certain circumstances; only the Pythagoreans forbade it absolutely. The same holds true for medically assisted suicide, a widespread practice in antiquity, and one opposed only by the Pythagoreans. Edelstein was led to the conclusion that the Oath is considerably influenced by Pythagorean ideas and teaching (Lypourlis, 2001, pp. 61-63), and indeed believed it to have been written by a doctor in Pythagorean circles. This explains in part why the Oath promotes a stricter medical ethic than that prevailing until then in ancient Greece, in Platonic and Aristotelian ethics, and also in daily medical practice. Doubts about authorship notwithstanding, the Hippocratic Oath was for centuries unquestionably the fundamental benchmark of medical ethics.
The Oath consists of two parts. The first defines the teacher-pupil relationship and the second is the code of ethics. In antiquity the teacher-pupil relationship possessed a marked ethical element. The closeness of the relationship and the deep understanding of the pupil’s personality built up during the long apprenticeship discouraged the entry of unworthy persons into this most important profession (Veatch, 1978, pp. 172-180).
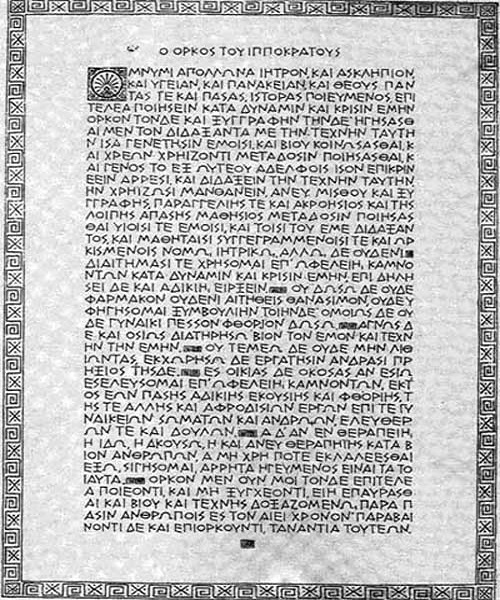
The present paper is of course chiefly concerned with the second part – medicine’s code of ethics. The oaths that the new physician swears by Apollo are the following:
1. He shall use his judgment to administer the best medical and medicinal treatment, only for the benefit for the patient επ’ ωφελείη.
2. He shall not, even if asked, give any deadly medicine nor advice to this end (of suicide).
3. He shall not induce an abortion.
4. He shall keep his life and his art pure and clean.
5. He shall not operate for a kidney stone (meaning he must not use techniques he does not know).
6. He shall refrain from knowingly causing injustice or harm.
7. He shall not have sexual relations with his patients.
8. He shall observe medical confidentiality (Konold, 1978, pp. 162-172).
A comparison with the relevant international bibliography is very revealing of the extent to which the Hippocratic Oath has influenced medical ethics throughout the ages. It is noteworthy that two of the four principles of bioethics, those of non maleficence and beneficence[5], which are considered to derive from Mill’s utilitarianism, are specifically mentioned in the Oath. (επ’ ωφελείη…εκτός πάσης αδικίης και φθορίης).
The emphasis laid on these principles implies an awareness that medicine can harm instead of heal, and that there may be physicians who would use their skill to harm rather than help.
The prevailing tradition in classical times promoted the image of a physician who looked healthy and had the right body weight, because, as Hippocrates quotes in his ‘Physician and Decorum’, the public believe that unfit physicians must be incapable of taking care of others.
Although the Hippocratic Corpus and more specifically the Oath is taken to reflect the standards of professional ethics of everyday Hellenic medical practice, some of its provisions are in sharp contrast to those standards. For instance, Hellenic medical practice allowed physicians to assist suicide and infanticide and to perform surgery, including lithotomy, all practices incompatible with the ethics of the Hippocratic Oath. Again, the Oath set high standards for the equal treatment of all social classes, standards not commonly attained in Greek society.
These precepts, representing the ideas of only a small group of medical practitioners, have outweighed all others in shaping the development of medical ethics in the modern world. But for centuries following the appearance of the Hippocratic Oath the medical profession showed no real respect for its provisions.
Hippocratic Ethics & Christianity
The major figure in ancient medicine after Hippocrates was Galen, a Greek from Pergamum. He lived in the second century A.D. and for most of his life in Rome as physician to the emperor and Stoic philosopher Marcus Aurelius. He himself left no writings on medical ethics. Despite his differences with his predecessor Hippocrates regarding his scientific methods, he is considered to have kept to the Hippocratic medical spirit. Given his reputed modesty and integrity and the fact that his medical techniques were not contrary to the Church’s views at that time (for example, he did not dissect dead bodies), he was especially liked in Christian circles and in a way acted as a bridge between Hippocratic medical ethics and the Christian attitude to medicine (Marketos, 2002, pp. 123-127).
The rise of Christianity produced a new idealism that was in general agreement with Hippocratic ethics. The increased attention paid to the Oath led to modifications that harmonized it with Christian ideological concepts and practices. The earliest of these revisions modifies the Hippocratic oath so that a Christian may take it (Leake, 1927), by replacing the references to Greek deities in the original oath with a Christian statement of worship of God. In addition it replaces the contract with a statement of the responsibilities that should be taught in a spirit of Christian brotherhood, which bind the physician to teach his art to whoever wants to learn it.
Christian anthropology (meaning here the study of man in his relation to God), which has given rise to the idea of human life having value and to ethics in general, is largely grounded in Jewish anthropology. It is thus noteworthy that manuscripts describing ancient Hebrew medical practices reveal Hippocratic influences in their prohibitions against administering poisons, committing adultery and disclosing professional secrets.
A later development of the above were the medieval Christian oaths, which instructed physicians to give special consideration to the poor and needy.
The Hippocratic Oath also appeared in medieval Muslim literature, where the only significant changes replaced references to Greek gods with statements complying with Islamic theology. It is believed that the Hippocratic Oath was taken by physicians practicing in both Christian and Muslim societies in the Middle Ages (Harakas, 1978, pp. 347-356).
With the establishment of the Eastern Roman Empire and the development of Byzantine civilization, the dominant trend in medicine became the so-called ‘Hippocratic Galenism’ (Marketos, 2002, p. 131). As a result the ethical rules of the Hippocratic Oath continued in force. No particular system of medical ethics appeared. However, historical references show that matters like the doctor-patient relationship, doctors’ social behavior and professional ethics concerned the Christian communities (Eutychiades, 1983, p. 7). Christian teaching seems to have infused the whole spectrum of medical treatment, going beyond even the moral rules of the Hippocratic Oath by taking charity as its guiding light. The first hospitals and almshouses appeared, under the auspices of important political and church leaders such as St Helen and Basil the Great. Hence Byzantium’s major contribution to medicine and nursing was the institution of the hospital and hospital care. This may be attributable to Christ’s command to love one’s neighbour (Marketos, 2002, 135), which together with love of God is considered the fundamental rule of Christian ethics (Mt. 22, 40. Mantzarides, 2004, p. 105). Thus Byzantium continued the ancient Greek tradition of developments in medicine following those in ethics.
It is important to stress the new meaning that Christianity gave to the human body through its anthropology, which derives from Christology. The prospect of salvation through participation in the Cross and the Resurrection reverses the approach to man as a solely biological unit. This inevitably reflects on the view taken of medicine. Christ’s voluntary death and Resurrection inspired the martyrs of the church and later ascetics to copy Him. Both kinds of saints have this in common, that they hold biological existence of less account than their love of Christ and hope of the resurrection. While not devaluing the body, they give it the opportunity to transcend the finite limits of this life. This leads the Church on the one hand to honour medicine as a science and the doctor’s role in relieving human suffering, but on the other to put it in perspective: Basil the Great states in his 55th rule that medicine should be used without its becoming an end in itself. Having himself studied medicine he knows its worth, but he points to the danger that man will forget his true vocation, which is eternal life, if he uses medicine to care for his body as an end in itself. This position is a rule that reflects the whole spirit of Byzantine civilization, a spirit that despite very great difficulties continued to be associated with the Greek world even after the fall of Constantinople in 1453 (Harakas, 1990, 9f).
The Hippocratic Oath in the modern era
The Hippocratic Oath continued to influence medical ethics in the West even after the Middle Ages gave way to modern Western society. Medical schools, seeking to commit their students to the pursuit of high ethical ideals, continued a tradition begun in the Middle Ages of incorporating Hippocratic concepts into oaths for their graduates, especially the covenant’s requirement for the physician to instruct his teacher’s children and the ethical strictures on confidentiality and the administration of harmful drugs.
From the 18th century onwards, and especially during the 19th century, many Greeks travelled to Western Europe to study medicine. There were medical-philosophical schools (e.g. at Padua) where in the spirit of the Enlightenment and the preceding Renaissance there circulated new ideas and attitudes to science in general and medicine in particular. These attitudes were brought to Turkish-occupied Greece and later into the newly-established modern Greek state by Greeks who had studied medicine abroad, among them important political figures such as Ioannes Capodistrias, Ioannes Kolettis and Alexandros Mavrokordatos, and also by men of letters like Adamantios Korais (Marketos, 2002, p. 397, p. 411, p. 413). Thus scientific thought in modern Greek society began to follow, and still follows, though slowly, Western scientific thought. Medical ethics is, of course, no exception to this development.
In Greece the Oath continues to be taken in its ancient form even today. However much it may be regarded as purely ceremonial, it cannot be entirely disassociated from the molding of a general ethic in relation to the medical profession. This is shown by the numerous references to the Hippocratic Oath in scientific congresses or studies whenever a question of medical ethics arises.
A significant revision of the of Hippocratic Oath appeared in 1948, when the newly organized World Medical Association (WMA) adopted the Geneva Declaration, a secular oath with no reference to religious tenets which attempts to make the original Hippocratic Oath fully applicable to modern conditions of medical practice and to diverse cultures[6].
However, the Declaration separates from the Hippocratic Oath the notions of gratitude to teachers and professional solidarity, extending them to embrace the profession on an international scale. In contrast its statement of the physician’s responsibility regarding suicide, mercy killing and abortion is carefully obscured in generalities, concealing modern controversy on these matters. It does, however, emphasise respect for human life from the moment of conception.
Recent biomedical advances and changing social demands have raised a number of new moral questions and dilemmas, for which the traditional ethical guidelines laid down in the Hippocratic Corpus are no longer adequate.
The Hippocratic Corpus, reflecting more or less the mores and ethos of classical Hellenic society, promoted a paternalistic attitude which made the physician the dominant party in deciding what was best for the patient. However, the other ethical values and principles established by the Hippocratic Corpus and its supporters in later centuries are still respected. In modern times society has challenged the paternalism of the Hippocratic Oath. This challenge, however, does not refute its historical and ethical value. On the contrary, it shows that there are timeless values that evolve in line with social changes.
The Hippocratic Tradition in modern Greece
The Hippocratic tradition has deeply influenced medical ethics and prevails even today in Greece (Hippocrates’s native land). This explains the frequently paternalistic attitude of Greek doctors; an attitude, moreover, that is accepted almost without question by patients, who often consider it perfectly normal. In fact, doctors in Greece care more for the well-being of their patients than for their rights. They are guided by the principles of beneficence, non-maleficence and paternalistic idea that physicians have the right to decide for their patients. Thus physicians do not usually inform patients and sometimes even take major decisions for them without their informed consent.
The concept of confidentiality is as highly valued in modern as in ancient Greece. The Hellenic Penal Code (section 371) punishes breach of medical confidentiality and exempts physicians from testifying in Court about what has been confided to them during the practice of their profession[7].
The Hippocratic tradition, in conjunction with the Greek Orthodox tradition, have deeply influenced Greek ethics and law. Euthanasia in any form, active or passive, is morally condemned and legally punished. However, recent medical advances have led modern Greek society to seriously question the ethics of keeping a terminally ill patient alive indefinitely. Therefore, “letting the patient die” as a form of passive euthanasia is under public discussion with a view to being accepted, under conditions, of course.
The issue of abortion in Greece raises several questions. Considering the religious and cultural background of Greece, there is an irony in the way Greek women contemplate abortion, since it is estimated that in the years before the legalization of abortion on request in Greece in 1986, 300,000 – 400,000 illegal abortions were performed annually,. We believe that socio-economic reasons, the feminist movement, lack of support for working mothers and large families led the state to legalize abortions. Artificial fertilisation has become to a great extent ethically acceptable even though it has only recently been subject to legislation[8]. The matter of transplants has been anticipated in a very similar way [9].
Bioethics in Greece
In recent decades a new discipline has made its appearance, initially in the USA: bioethics, which we have already mentioned at the beginning of this paper. Bioethics is a child of the rapid advances in biomedical research and applications and especially genetic technology, and chiefly concerns societies that have been pioneers in this field. Greek society, despite its distinguished scientific community, is a consumer of biomedical technology rather than a participant in research and production. As a result the bioethical problems are imported along with the technology. This creates a somewhat complicated situation. Bioethical problems, apart from biomedical applications, have their origin in what is defined as spirit in Western culture. The factors that comprise the prevailing moral attitude in Greek society derive on the one hand from Western culture and on the other from the Eastern Orthodox Christian Tradition. The latter, however, differs fundamentally at many points from the Western spirit. This means that bioethics, which reflects the moral outlook of another, though not completely alien, culture, cannot be called upon to solve the bioethical problems that arise in Greek society in exactly the same way it would in the culture that gave birth to it.
Bioethical issues began cautiously to be raised in Greece in the 1980’s[10]. The academic community’s interest in the subject showed itself first sporadically in university lectures and more rarely in papers. The public learnt about it only through a few articles in the press. The situation changed considerably, however, in the following decade. It could be argued that interest in bioethics increased as the project to decode the human genome neared completion. Newspaper articles multiplied, academics began to take positions by publishing papers, and congresses, workshops and lectures on bioethical issues were organised. These congresses and the interdisciplinary cooperation they encouraged laid the groundwork for the creation of bioethics committees. Finally at the turn of the century the first official bioethics committees were set up in Greece, although they are only of an educational and advisory character. The most important of these are the National Bioethics Committee (under the auspices of the Prime Minister)[11], the Bioethics Committee of the General Secretariat of Research and Technology of the Ministry of Development[12] and the Ethics and Deontology Committee of the Ministry of Health.
At the academic level, bioethics has begun to be taught as an elective subject in the relevant university schools, such as those of medicine, biology, philosophy, theology and law. Postgraduate and doctoral theses have been written on the subject and in the last two years the University of Crete has established an interdepartmental program of postgraduate studies in bioethics[13].
The Church of Greece has also made a significant contribution by setting up a special bioethics committee of the Holy Synod[14]. Another important initiative is the foundation of the first Center of Biomedical Ethics and Deontology[15] by the then archimandrite and now metropolitan of Mesogaia and Lavreotiki Nikolaos Hadjinikolaou.

Metropolitan of Mesogaia and Lavreotiki Nikolaos
Bioethics and Orthodox tradition
In the Eastern Orthodox tradition, ethical practices are those that conform to the ethics of the Orthodox faith. There is nothing in Christian Orthodox teaching that overtly or covertly opposes or even expresses reservations about the art of medicine. Even when it is canonical in character it is not stated in a rigid, legalistic or absolute manner. Dispensation (in theological terms “economia” – a form of conditional concession) authorizes an exception to the rule, without, however, treating it as a precedent or as abrogating the rule. The justification for a dispensation is the avoidance of the greater harm that would result from strict application of the rule (Kalliakmanis, 2000, p. 73).
The doctrinal teachings of Orthodoxy are directly applicable to medical ethics and bioethics. Of particular importance is Orthodox anthropological teaching, which derives from the creation of man ‘in the image and likeness’ of God, as a unity of body and soul and from Christological doctrine. Eastern Orthodox ethics are based on honor and respect for each individual life from the moment of conception. This can be clearly seen in the church calendar, which honors the great feasts of the Annunciation (the conception of Christ), the conception of the Virgin and the conception of John the Baptist. Thus the birth of every single human being, who is created in the image of God, should be treated as a great event, as a feast. Hence Orthodox theology regards life as a gift from God and demands that it be treated with proper respect and solicitude.
Any form of disrespect to human life, from abortion to euthanasia and from cloning and eugenic gene intervention to mercy killing or failure to give proper treatment to a needy patient, constitutes a violation of the main principle of orthodox bioethics, that of the Person-Hypostase (Koios, 2003, p. 256, p. 351). However, our religious tradition is not completely inflexible in these matters.
Dispensations are always granted under the guidence of a spiritual father, never arbitrarily. The dispensation has above all a spiritual purpose. It is not an exemption from the articles of faith, but a considered, temporary deviation from the strict implementation of the commandments, to prevent the wayward Christian from leaving the Church. The purpose of this concession is to overcome a particular difficult situation with the least possible cost.In this spirit, abortion has sometimes been permitted when the mother’s life is in danger. Even in this case, however, the main operative value is the protection of life and the balancing of numerous factors.
Sexuality and productivity are issues of great concern for Orthodox bio-ethicists. The Orthodox Church teaches that human sexuality is a divinely given dimension of human life that finds its fulfillment in conjugal relations. Hence artificial insemination techniques are acceptable provided the sperm donor is the husband. Even this case, however, raises ethical questions. The mechanisation of the mystery of life that results from removing the reproductive process from the warm environment of the womb to the cold surroundings of the laboratory and its consequences for family unity are major issues for Orthodox ethics.
Conclusion
After a brief flashback in history we can conclude to the following remarks:
- Although the oath itself is not part a certain ethical theory, it has been widely accepted in Greece as a basic text of Medical Ethics
- The principles of beneficence and non – maleficence and the protection of life of the embryo has been the common ground of the oath and the Christian Ethics. This common ground has resulted to the incorporation of the oath to the Christian teachings regarding Medical Ethics. The oath together with Christian anthropology have ever since been the bases of the East Orthodox Church, for the ethical evaluation and approach of every question regarding Medical Ethics and Bioethics.
- The work of Galen has further reinforced the spirit of the Hippocratian Medicine in Greece regarding both Medicine and Medical Ethics.
- The transport of the humanitarian ideas of the Enlightenment with the Hippocratian Ideas and the Christian principles have formed the framework of the modern ethical perception of Medical Ethics and Bioethics in Greece.
- The Hippocratian Ethics have formed the two basic principles of Bioethics mentioned above. In Greece its influences can been found to the Medical Paternalism that still survives even today.
Epilogue
After the second world war, Greek society to a great degree followed the social, political, economic and scientific developments in the West. Most of the scientists at the forefront of medical progress in Greece studied in Western Europe or the USA, and thus brought a western outlook to questions of medical ethics and deontology. These are laid down in international treaties and conventions such as those of Geneva, Helsinki and Oviedo, in national legislation and by the academic community in each individual medical school.
However, medical ethics in the West is based on the Western ethic: Western humanism and all it involves. The modern, dominant attitude to ethics is expressed in everyday medical practice though the promotion of the rights of the individual, in this case the patient. Although Greek society has not remained untouched by these developments, it cannot yet claim to be moving steadily towards a less paternalistic approach to medicine. The reasons are many and chiefly have to do with the attitude of the Greek community to the medical profession, but also our cultural background, which differs from that of the West. This is a major issue of medical ethics and education, which will have a considerable influence on the doctor-patient relationship, as has already happened in other societies.
Although is argued that Greek patients lack sophistication and cohesiveness in the doctor-patient relationship, additional studies are needed to assess the sensitivities and needs of the Greek population to issues related to health and its social aspects.
As we look ahead, we are optimistic about our culture’s abilities to guide the practice of medicine in ethically acceptable ways. It is especially encouraging that bioethics committees have been established by various bodies, such as ministries, scientific institutes and the Church. Greek culture, grounded as it is in ancient Greek thought on the one hand and the Orthodox Christian tradition on the other, clearly possesses both dynamism and flexibility, and also timeless ethical values. Experience has shown that in Greece ethics have always been both a matter of debate and in a state of evolution.
Adjustment to the new European and also global reality can take place through constructive dialogue between institutions and society. It is essential that the public is well informed, so that it is in a position to debate the ethical challenges posed by scientific advances rather than to passively accept them. The fact that Western societies, despite their considerable differences, have to a great extent the same cultural roots as Greek society, the ancient Greek world and Christianity means that it will be possible to find points of agreement and a common approach to the ethical problems raised by the practice of medicine and especially modern medicine.
Such an approach to the understanding of ethical problems associated with medical practice may provide, after in-depth analysis of the inevitable cultural differences, a precedent for ethical problem-solving within each nation (Veloyanni – Moutsopoulou & Bartsocas, 1989, pp. 209-234).
Bibliography
Ammudsen D. W. & Ferngren, G. B. (1983). Evolution of the Patient-Physician Relationship: Antiquity Through the Renaissance. In E. A. Shelp (Ed.) The Clinical Encounter: The Moral Fabric of the Patient-Physician Relationship (pp. 1-46). Dordrecht, The Netherlands: D. Reidel Publishing Co.,
Beauchamp, T. L. (1993). The Principles Approach. Special Supplement, Hasting Center Report 6.
Edelstein, L. (1943). The Hippocratic Oath: Text, translation & interpretation. Baltimore: Johns Hopkins Press.
Eutychiades, A. (1983). The practice of Byzantine medical science and its social applications according to relative provisions. (Η άσκησις της Βυζαντινής ιατρικής επιστήμης και κοινωνικαί εφαρμογαί αυτής κατά σχετικάς διατάξεις), (Greek ed.). Athens: Κ. Παρισιάνος.
Harakas, S. (1978). Eastern Orthodox Christianity. In Encyclopedia of Bioethics (pp. 347-356), New York: McMillan.
Harakas, S. (1990). Health and Medicine in the Eastern Orthodox Tradition. New York: Crossroad.
Jones, W. H. S. (1924). The Doctor’s Oath. The Early Forms of the Hippocratic Oath. New York: Cambridge University Press.
Kalliakmanis, V. (2000). Girded with the Towel: Methodological presuppositions of Pastoral treatment (Λεντύω Ζωννύμενοι: Μεθοδολογικά πρότερα Ποιμαντικής), (Greek ed.). Thessaloniki.
Koios, N. (2003). Ethical review of the artificial intervention in the human genome (Ηθική θεώρηση των τεχνικών παρεμβάσεων στο ανθρώπινο γονιδίωμα), (Greek ed.). Athens: Center of Biomedical Ethics and Deontology.
Konold, D. (1978). Codes of Medical Ethics (History). In Encyclopedia of Bioethics (pp. 162-172). New York: McMillan.
Korff, W. (1998). Einfürung in das Projiect Bioethik, In Lexicon der Bioethik (vol. 1, pp.7-16). Güttersloh.
Leake, C. (1927). Percival’s Medical ethics. Baltimore: William & Wilkins.
Lypourlis, D. (2001). (translation, introductions, comments), Hippocrates, Medical Deontology and Nosology (Ιπποκράτης, Ιατρική δεοντολογία και Νοσολογία), critical edition, Thessaloniki: Ζήτρος.
Mantzarides, G. (2004). Christian Ethics II (Χριστιανική Ηθική ΙΙ), (Greek ed.), Thessaloniki: Πουρναράς.
Marketos, Sp. (2002). History of Medicine (Ιστορία της Ιατρικής). Athens: Zήτα.
Veatch, R. W. (1978). Codes of Medical Ethics (Ethical Analysis), In Encyclopedia of Bioethics (pp. 172-180). New York: McMillan.
Veloyanni – Moutsopoulou L., & Bartsocas C. S. (1989). “Ethical and Medical Genetics in Greece”, In D. C. Wertz, & J. C. Fletcher (Eds.). Ethics and Human Genetics: A Cross-Cultural Perspective (pp. 209-234). New York: Springer-Verlag.
Veloyanni – Moutsopoulou, L. (1984). Ethical and Social Health Policy (Ηθική και Κοινωνική Πολιτική Υγείας). Ioannina.
[1] Nikolaos Koios is a Doctor of Theology with specialization in the fields of Christian Ethics and Bioethics. He works as a public school teacher of religion in Secondary Education. He has specialized in Ethics and Bioethics at the Faculty of Theology of the Aristotele University of Thessaloniki, Ludwigs Maximillian University of Munich and the Hasting Center in New York.
[2] Dr. Lambrini Veloyanni is Associate Professor at the School of Medicine at the University of Ioannina. She teaches Medical Ethics, Bioethics, Deontology of Medicine and History of Medicine. She has specialized in Bioethics at the Kennedy Institute of Bioethics in Washington DC.
[3] Demetrios Alvanos is Attorney at Law appointed to the Court of Appeals. He has done postgraduate studies in Human Rights at the University of Padova and the University Centre of Luxemburg.
[4] It is wrong to use the term “bioethics” instead of the term medical ethics, especially for antiquity. Bioethics is a product of modern society, having arisen from the use of biotechnology and the ethical problems the latter has created. For further information see (Korff, 1998, p. 7).
[5]The other two are autonomy and justice (Beauchamp, 1993).
[6] Declaration of Geneva, Declaration of Helsinki, Declaration of Sydney, Declaration of Oslo, New York: W.M.A.
[7] Greek Penal Code, 11/ 17-8-1950.
[8] Law N.3305.2005
[9] Law N. 2737.1999
[10] When one of the first doctoral theses on bioethics was submitted. (Veloyanni – Moutsopoulou, 1984.)
[11] For further information see www.bioethics.gr
[12] For further information see www.gsrt.gr
[13] For further information see www. bioethics.fks.uoc.gr
[14] For further information see www.ecclesia.gr/greek/holysynod/commitees/bioethics
[15] For further information see www.bioethics.org .gr